Restorative dental materials are used to prevent or repair damage to teeth caused by oral disease or trauma. Though the currently available restorative materials like glass ionomer cements, resin restorations etc may serve the purpose by restoring the form and function of the tooth but lacks the bioactivity. Secondary caries caused by polymerization shrinkage and micro leakage are other major contributing factors for the failure of restorations.


DentoClude™ F contains Bioactive glass which promotes remineralization of the demineralized enamel. Demineralization of teeth occurs when an acidic by-product of plaque wears away the enamel of the teeth. When a tooth is subjected to tooth decay, the minerals such as calcium and phosphate in the tooth begin to wear away hence “demineralization” and make the enamel in the tooth porous, sometimes leading to cavities or other dental issues. The standard of care to treat early caries lesions like White Spot Lesions (WSLs), regular plaque removal and fluoride application. Recently, phosphopeptide-amorphous calcium phosphate (CPP-ACP) is also used as an alternate therapy.


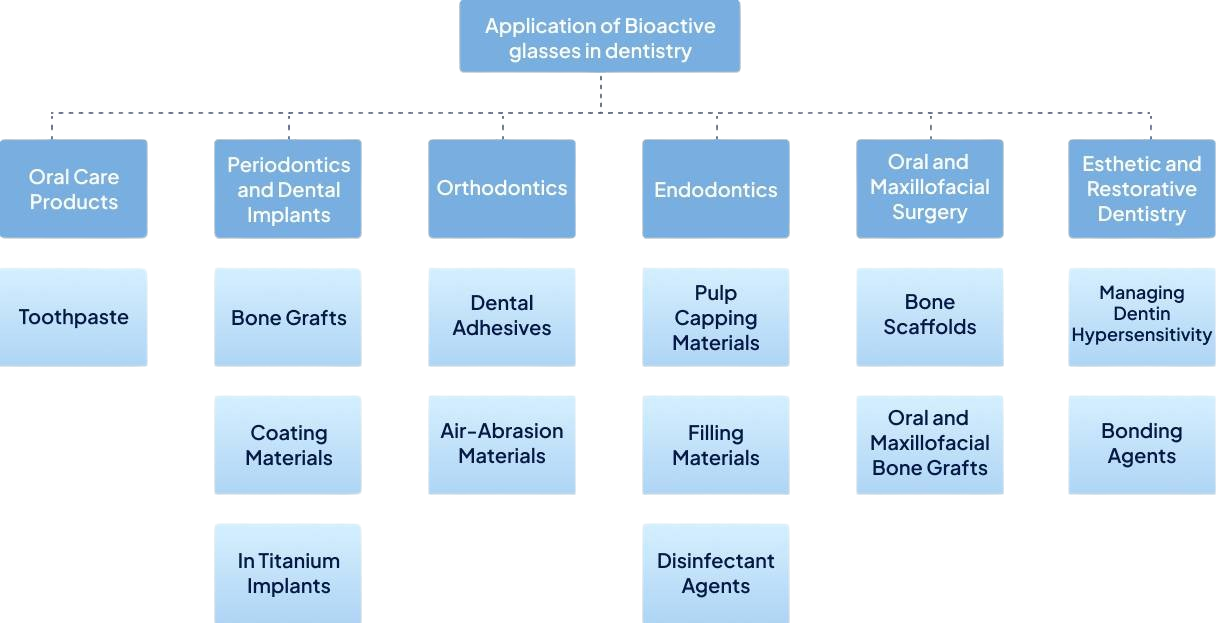
DentoClude™ F has Bioactive glass as an active ingredient which is a clinically proven and well accepted oral tissue regenerative material. Bioactive glass has the ability of bonding to hard and soft tissues without rejection. They are osteoinductive, stimulate the proliferation of bone cells, and also are totally resorbable. The particle size of bioactive glass in DentoClude™ F being less than 1micron aids in coating the dental implant surfaces that promotes remineralization to create stronger post implants etc. Additionally, DentoClude™ F formulation is comprised of botanical excipients to prevent anti-inflammation/ infections.






Jafari, N., Habashi, M.S., Hashemi, A. et al. Application of bioactive glasses in various dental fields. Biomater Res 26, 31 (2022). https://doi.org/10.1186/s40824-022-00274-6


Neeraja Govindaraj, Kinjal Shah Virani, Priya Subramaniam, Megha Gupta. Evaluation of bioactive glass and hydroxyapatite crystals as pulpotomy agents in primary molars: A clinical study. Contemp Pediatr Dent 2020:1(1):42-51.
Skallevold HE, Rokaya D, Khurshid Z, Zafar MS. Bioactive glass applications in dentistry. Int J Mol Sci. 2019;20:5960.
Dr. Abinaya R, Dr. Pallavi Urs, Dr. Priya Nagar, Dr. Arul Selvan, Dr. Smitha S, Dr. Janani J. Comparative evaluation of antimicrobial efficacy of bioactive glass, 1% chlorhexidine gluconate with calcium hydroxide and 1% chlorhexidine gluconate, as intracanal medicament in primary molars: An in vivo study. Int J Appl Dent Sci 2021;7(4):82-88. DOI:https://doi.org/10.22271/oral.2021.v7.i4b.1355.

Profeta, Andrea Corrado and Christoph Huppa. “Bioactive-glass in Oral and Maxillofacial Surgery.” Craniomaxillofacial Trauma & Reconstruction 9 (2016): 001 – 014.
At DentoClude™ F, we innovate dental solutions to enhance patient care. Our flagship product, DentoClude™ F, offers cutting-edge technology for effective tooth sensitivity relief.
© 2024, DentoClude™ F, All Rights Reserved, Powered by Kerlotech.